Advance Response, LLC
Automated Healthcare Claim Research & Analytics Portal
Private Fundraise
This company may be interested in raising funds from accredited investors. You must Request Access to see more information about this company.
Request Access 9

Quick Pitch
Although aggregated research portals have proliferated across other industries like news and travel, a void has remained in healthcare claim research. Medical billers primarily spend their time in research or resolution, and the more time spent researching takes away time from resolving. Typically, billers spend at least 5-10 minutes (or more) to manually research the status of a claim across different insurance web sites and/or via phone calls, which limits productivity that would otherwise be put toward resolution and driving reimbursement revenue.
Advance Response has now built and deployed a cloud-based automated claim research & analytics solution; our research algorithms are best-in-class, and coupled with scalable automation, can drive unprecedented productivity and insightful analytics:
- Billing groups increase net productivity by 30%+.
- Automatically researches multiple payers @ 1000's of accounts/hour!
- Advanced research algorithms increases "find" rates (avoids 20% biller effort finding nothing)
- Standardized interface enables billers to see claims across payers in a single view.
- Powerful data analytics tools quickly filters, sorts and prioritizes workflow.
- Transforms research time into resolution and drives revenue velocity!

Product/Service Details
The Advance Response Solution includes compiling the following detailed medical claim information:
- Interactive, comprehensive search algorithms automate the claim research process: "If a claim exists, we'll find it! If it doesn't exist, we'll save you the time of NOT finding it!"
- As part of a comprehensive claim research process, eligibility can be confirmed and complements the claim status info.
- Multi-channel research capabilities--no more navigating web sites and/or sitting on hold.
- Business rules driven, granular claim status leverages predictive next-step action: "custom status policies not only give you the payer's status, but what to do next."
- Detailed, methodical data-discrepancy analysis highlights data fields where provider and payer information isn't consistent, thereby leading to faster reconciliation and resubmittal.
- Automated notes: billers no longer have to type (or typo) notes to capture the findings and/or phone discussions with payers. Categorized notes become sortable--analytics offer trending insights across providers, payers, and billers.
- Web-based URL for integrating the return file output into other software vendor environments.
- Insightful reports lend unprecedented insight into ways to transform the billing research and resolution process!
How We're Different
Unlike most healthcare software vendors who primarily address the initial claims submission process, Advance Response focuses on claim follow-up research to drive resolution.
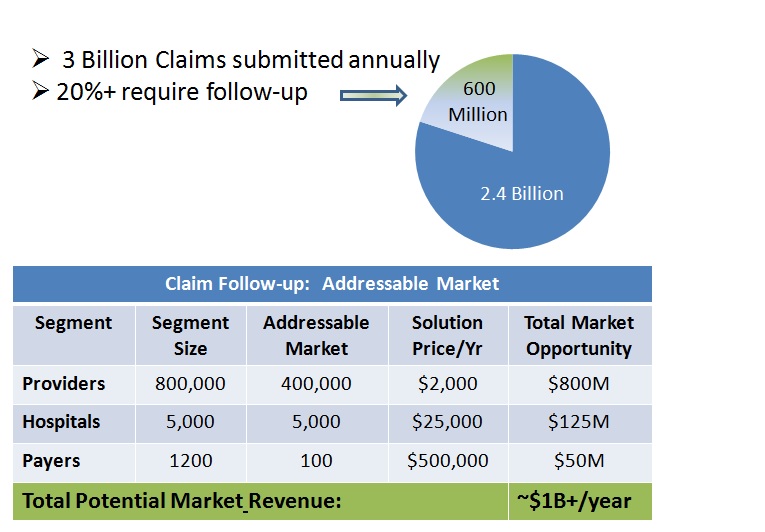
Consistent with the 80/20 rule, 20% of submitted medical claims...or about 600,000,000 claims industry-wide, require some sort of follow-up, but drive about 80% of the work. The Advance Response solution uniquely aggregates medical claim data--and presents this data in a first-of-its kind, filter-and-sortable interface for refining workflow next steps using predictive, data-driven analysis.
Traction & Accomplishments
- Developed and deployed a cloud-based production platform for automating claim research - over 25,000 claims processed as of April 2013.
- Four (4) patent applications filed & pending.
- Currently deploying solutions with 3 golden clients:
- Large outsourced billing services company, handing provider and hospital emergency department clients in California and Arizona.
- Major hospital client and its healthcare software vendor in New Jersey.
- Medical billing services provider in New Jersey, providing outsourced billing services for a large hospital.
The Business Plan area is locked. You must Request Access to this company to see more information including the Business Plan.
Request Access
N
No updates yet.
%
No backers yet.
Quick Signup TBD
You must have an account to do this!
